Table of contents
- The significance of a healthy gut
- Gastrointestinal infections: Causes and consequences
- How to prevent gastrointestinal infections
- Treatment of gastrointestinal infections
- How to restore gut health after gastrointestinal infections
- The right nutrition to restore your gut flora
- Probiotics and prebiotics for gut health
- How gut flora regeneration works at the microbial level
- Conclusion
The significance of a healthy gut
Your gut hosts trillions of microorganisms, predominantly bacteria. Together, they constitute your unique gut microbiome, or gut flora. A healthy gut flora is characterized by a high diversity of bacteria and serves as the foundation for our health and well-being, playing a crucial role in numerous bodily functions. Beyond aiding digestion, these microorganisms also have a significant impact on your immune system and mental health.
Gastrointestinal infections can disrupt the balance of your gut microbiome, leading to a range of health issues. Research has linked these imbalances to digestive problems, inflammatory bowel diseases, diabetes, skin conditions, and allergic reactions, among others. When your gut health is compromised, you may struggle to absorb essential nutrients, and harmful substances can enter your body more easily. Moreover, potentially pathogenic bacteria can thrive under these conditions (1,2).
In this blog post, you'll discover why it's essential to prioritize your gut health following a gastrointestinal infection and receive practical tips on restoring the balance of your gut flora.
Gastrointestinal infections: Causes and consequences
A gastrointestinal infection, often colloquially referred to as "stomach flu", bears little resemblance to the actual flu. Rather, it's an inflammation of the mucous membrane that lines the stomach and intestines. Typically, these infections are triggered by microorganisms such as bacteria, viruses, or parasites. Transmission often occurs from person to person, primarily through direct or indirect contact with contaminated fecal matter. Food poisoning, caused by consuming contaminated food or water, is also a common source of these infections. Even swimming in contaminated water can lead to the ingestion of certain pathogens.
The primary culprits behind gastrointestinal infections are usually rotaviruses and noroviruses. When bacteria are the cause, they are often specific strains of Escherichia coli, Campylobacter, Shigella, Salmonella, Clostridioides difficile, and Staphylococci. Some bacteria invade the intestinal lining directly, causing cellular damage, while others produce toxins that induce gastrointestinal symptoms (3).
Interestingly, only a minority of bacteria consistently cause illness upon infecting the body. In fact, 99% of all bacteria are harmless and play vital roles in maintaining our health (1). For those interested in delving deeper into the functions of key bacteria, our blog posts "The Basics of Gut Bacteria – Part I" and "The Basics of Gut Bacteria – Part II" offer valuable insights.
Symptoms of gastrointestinal infections include sudden-onset diarrhea, nausea, vomiting, abdominal cramps, and pain, and in more severe cases, fever, general malaise, and muscle aches. The nature and severity of symptoms hinge on the type and quantity of the pathogen or toxin encountered. While the infection is generally mild in healthy adults, it can pose life-threatening risks, particularly in children, the elderly, or individuals with compromised immune systems, due to severe dehydration and electrolyte imbalances (3).
In any event, a gastrointestinal infection disrupts the equilibrium of your gut microbiome, making it difficult for beneficial bacteria to maintain their presence and function effectively.
How to prevent gastrointestinal infections
The most effective measures to prevent gastroenteritis include meticulous kitchen hygiene and frequent, thorough handwashing. Additionally, long-term care of your gut microbiome plays a crucial role in prevention. A healthy gut flora is less susceptible to pathogens, supports a robust immune system, and is associated with milder and shorter durations of gastrointestinal infections (4).
Wondering what proper care for a healthy gut microbiome entails? Diet plays a significant role, which we'll delve into in more detail below. Furthermore, managing stress, engaging in regular physical activity, getting adequate sleep, and avoiding toxins such as alcohol are all crucial factors. For more details, check out our 5 Steps to a Healthy Gut Microbiome guide.
Treatment of gastrointestinal infections
The cornerstone of treating a gastrointestinal infection is maintaining adequate hydration. Vomiting and diarrhea lead to significant loss of fluids and electrolytes such as sodium, potassium, calcium, and magnesium. Special electrolyte solutions or water combined with a pinch of salt and sugar can help restore these imbalances. In some cases, healthcare professionals may also prescribe medications to alleviate nausea or stop diarrhea (3).
Antibiotics are another treatment option, but they are only effective against bacterial infections. They offer no benefit against viral or parasitic infections and can be an additional burden to your digestive system. Improper use of antibiotics can lead to antibiotic resistance. Additionally, antibiotics can disrupt the healthy balance of the gut flora, as they not only kill harmful bacteria but also beneficial ones. This disruption can promote the growth of Clostridioides difficile bacteria, which often cause diarrhea. Furthermore, the choice of antibiotic is crucial for treatment success; depending on the bacterial species causing the infection, different antibiotic treatments are necessary (3,5).
An alternative treatment method to antibiotics, especially for infections caused by the bacterium Clostridioides difficile, is fecal microbiota transplantation (FMT). You can read more about this treatment method in our blog post: Fecal Transplantation – A Promising Treatment For Clostridioides.
Easy-to-digest foods to support your digestive system
As the most severe symptoms of a gastrointestinal infection begin to wane, transitioning to a balanced, gentle diet is recommended to replenish the body's energy levels. This diet should include easily digestible foods that are also nutrient-dense.
If you're experiencing diarrhea or vomiting, consuming multiple small meals throughout the day can be beneficial. Salted oatmeal soup or vegetable broth are gentle on the stomach and can help replenish lost electrolytes. Gradually reintroduce solid foods as your symptoms improve. While it's important to eat what feels right for you, it's advisable to avoid of fatty and sugary foods, as well as carbonated drinks, ice-cold beverages, alcohol, and nicotine (6).
Here are some recommended foods for a gentle diet during a gastrointestinal infection:
- Fruits: Opt for easily digestible fruits like apples and bananas, ideally grated or pureed to ease digestion.
- Vegetables: Steamed vegetables or soups are easier to digest compared to raw ones. Vegetables like carrots, celery, parsnips, pumpkin, zucchini, and potatoes are well-tolerated. However, cabbages, onions, leeks, garlic, mushrooms, chili peppers, and legumes can be hard to digest.
- Grains: While whole grains are generally recommended, opt for refined, finely ground bread, pastries, and pasta when following a gentle diet. Day-old bread and rolls are also easier on the stomach. Crackers, oatmeal, rice, millet, couscous, and polenta are good alternatives
- Animal Products: Choose lean, mild cheeses and dairy products, as well as lean meats and fish.

Fact Check: Does Coca-Cola Really Help with Gastrointestinal Infections?
Many believe that Coca-Cola is a top-notch home remedy for gastrointestinal infections. Time to dispel this myth! Cola is high in sugar and low in essential minerals, making it more of a burden on the digestive system rather than a helpful solution (6).
How to restore gut health after gastrointestinal infections
To restore your gut flora after a gastrointestinal infection, it's essential to nourish your gut bacteria with the right food. While taking pre- and probiotics as supplements may aid in microbiome recovery, the research on their effectiveness is still inconclusive and varies based on individual factors. Alongside proper nutrition, getting enough rest and quality sleep are vital for a speedy recovery. Did you know that stress and sleep deprivation can negatively impact your gut flora? This is due to the interconnected communication between the gut and the brain (7).
The recovery time for your gut flora depends on the severity of the infection and your overall health. Studies indicate it may take anywhere from a few weeks to several months (8). So, patience is essential!
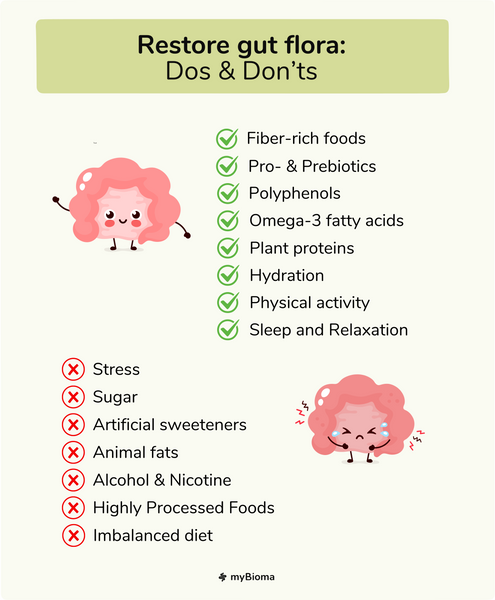
The right nutrition to restore your gut flora
A gut-supportive diet revolves around including plenty of fiber-rich foods that gut bacteria love. Fiber gets transformed by your gut bacteria into short-chain fatty acids, which play a key role in protecting the intestinal lining and maintaining overall health (11).
Tip: Amp up your fiber intake by choosing whole grains and incorporating a variety of vegetables, fruits, legumes, nuts, and seeds into your meals.
In addition to fiber, polyphenols, secondary plant compounds, are essential for a thriving microbiome. The more colorful and diverse your diet, the better! Healthy fats, especially omega-3 fatty acids, and plant-based proteins also contribute to a healthy gut (9). For more insights, explore our blog post: How Gut Bacteria Aid Digestion. Prebiotic and probiotic foods are crucial too, as they help beneficial bacteria flourish and establish themselves in the gut.
On the flip side, there are foods that can compromise gut health, such as animal fats, sugar, alcohol, and certain additives and artificial sweeteners (9,10).
Probiotics and prebiotics for gut health
Simply put: Probiotics are live bacteria that can enhance the diversity of your gut microbiome. Prebiotics serve as food for your gut bacteria. Both can be incorporated into your diet as foods or taken as dietary supplements.

Probiotics
Probiotics play a multifaceted role in your body, aiding in the restoration of a healthy gut microbiome. These live bacteria support your immune system, produce beneficial compounds like organic acids and antimicrobial agents, collaborate with other beneficial gut bacteria, reinforce your intestinal barrier, and generate essential enzymes crucial for various bodily functions (12).
Probiotic-rich foods include natural yogurt, buttermilk, kefir, aged cheeses, kombucha, miso paste, and fermented vegetables such as sauerkraut and kimchi. When selecting these items, opt for natural, unpasteurized versions or try making them at home. We have curated some great recipes for you:
- The health benefits of kefir and how to make it yourself
- Simple Kimchi Recipe: Fermented foods for better gut health
- Fermented Red Cabbage
Several studies suggest that consuming fermented foods can positively impact gut health and help restore microbiome balance (13,14). However, the efficacy depends on various factors and isn't always conclusively proven. Beyond their probiotic properties, fermented foods offer additional health advantages, making them a reliable health booster: The fermentation process enhances the digestibility of these foods and improves nutrient absorption. Additionally, they are rich sources of essential vitamins and minerals (14).
Probiotics can also be consumed in supplement form, such as pills or powders. However, many commercially available products lack verified efficacy, so it's essential to be cautious when choosing them. The seemingly straightforward approach of replenishing lost gut bacteria with supplements isn't as simple as it sounds. Probiotics don't necessarily contain the same bacteria lost during gastrointestinal infections or antibiotic treatments. The effectiveness of probiotics in aiding recovery after a gastrointestinal infection varies depending on the specific pathogen and the bacterial strain in the supplement. While some studies have demonstrated positive outcomes, the overall research is still insufficient and requires further exploration to ensure consistent therapeutic results (15,16).
Prebiotics
Prebiotics are specific types of fibers, such as inulin, oligofructose, and pectin, that serve as food for your beneficial gut bacteria, positively influencing the bacterial composition in your intestines. Among other benefits, they contribute to protection against pathogens, support your immune system, and enhance your digestion and mineral absorption (1,12).
Some examples of prebiotic foods include (17–19):
- Certain vegetables like chicory, salsify, Jerusalem artichokes, asparagus, leeks, and onions
- Some fruits like bananas, apples, and plums
- Oats, wheat, barley, and rye
- Legumes such as soybeans, peas, lentils, and beans
Tip: Resistant starch is a unique type of prebiotic fiber formed when starchy foods are cooked and then cooled. Potatoes, legumes, rice, and grain products can offer additional health benefits through this type of preparation (19).
Prebiotics can also be consumed as convenient supplements in the form of capsules or powders. However, the quality of these products can vary widely, so it's essential to research thoroughly before making a purchase.
The extent to which prebiotic foods and supplements can actually aid in the regeneration of your gut flora is not yet fully understood. Nonetheless, some studies indicate a protective effect of prebiotics against infection- or antibiotic-induced diarrhea, potentially reducing its duration (11).
How gut flora regeneration works at the microbial level
In cases of microbiome imbalance, such as after a gastrointestinal infection or antibiotic therapy, bacteria employ various strategies to combat pathogens and restore balance in the gut. These intricate interactions between microorganisms and the human body remain complex and not fully understood (20).
Here are some of the known mechanisms possibly involved:
1. Non-pathogenic bacteria can attach to pathogenic bacteria, making it more challenging for them to infect the body.
2. Certain bacteria can produce a protective barrier that prevents pathogens from adhering to mucous membranes and causing harm.
3. Some bacteria generate substances that can kill or weaken pathogens, akin to the antibodies our immune system produces.
4. Bacteria communicate with one another, emitting signals that suppress or reduce the production of harmful substances by pathogens.
5. Beneficial bacteria compete with harmful bacteria for nutrients and space, making survival difficult for the detrimental bacteria.
6. Bacteria influence the immune system, encouraging the production of substances that combat pathogens.
7. Certain bacteria support the integrity of "tight junctions," which are cell-to-cell connections regulating the permeability of the intestinal lining. This allows bacteria to prevent pathogen entry and minimize damage to the gut lining.
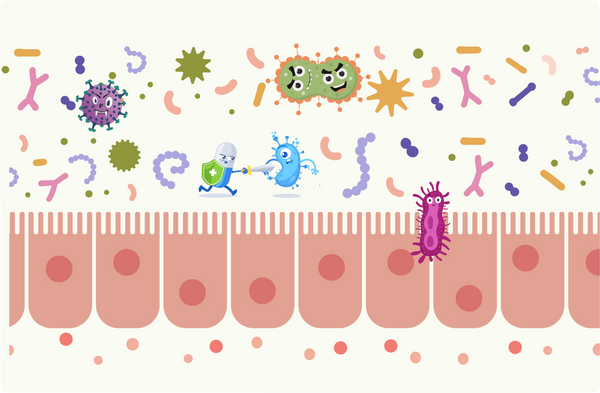
Beneficial bacteria outcompete and eliminate pathogens, safeguard the intestinal lining,
and bolster antibody support antibodies.
As you can see, establishing a healthy gut flora is a multifaceted process that can't be accomplished solely through individual mechanisms. For example, certain bacterial strains may serve beneficial roles in a healthy gut environment but might not offer the same advantages under disrupted conditions. Conversely, potentially harmful bacteria can sometimes have beneficial effects. It's all about the interplay and balance! Additionally, the regeneration process is influenced by various factors, including the initial composition of your microbiome, genetics, environment, diet, and the type and amount of pathogen encountered (20).
Conclusion
After a gastrointestinal infection, your gut flora is thrown off balance. To restore your gut health, adopting a gut-friendly lifestyle is essential. This includes getting enough sleep, managing stress effectively, engaging in regular physical activity, maintaining adequate hydration, and consuming a diverse, healthy diet rich in fiber and fermented, probiotic foods.
Have you recently recovered from a gastrointestinal infection and want to know the current state of your gut microbiome? With a myBioma microbiome test, you can easily gain insight into the health of your gut flora—based on scientific research and the latest technologies. Additionally, you'll receive personalized lifestyle and dietary recommendations to help improve your health and well-being. Order your microbiome test here.
References
- Bäckhed F, Fraser CM, Ringel Y, et al. (2012). Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe. 12(5):611–22.
- Salem I, Ramser A, Isham N, et al. (2018) The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front Microbiol. 9:1459.
- Gotfried J (2023) Übersicht über Gastroenteritis. MSD Manual Ausgabe für Patienten. Verfügbar unter: https://www.msdmanuals.com/de/heim/verdauungsst%C3%B6rungen/gastroenteritis/%C3%BCbersicht-%C3%BCber-gastroenteritis [zitiert am 5. April 2024]
- Lawley TD, Walker AW (2013) Intestinal colonization resistance. Immunology. 138(1):1–11.
- Suez J, Zmora N, Zilberman-Schapira G, et al. (2018) Post-Antibiotic Gut Mucosal Microbiome Reconstitution Is Impaired by Probiotics and Improved by Autologous FMT. Cell. 174(6):1406-1423.e16.
- Österreichische Gesundheitskasse (2020) Ernährung. Leichte Vollkost. Ernährungsempfehlungen für Leber, Magen, Darm & Galle. Gesundheits-Informations-Zentrum. Verfügbar unter: https://www.gesundheitskasse.at/cdscontent/load?contentid=10008.721329 [zitiert am 12. April 2024]
- Han M, Yuan S, Zhang J. (2022) The interplay between sleep and gut microbiota. Brain Res Bull. 180:131–46.
- Ng KM, Aranda-Díaz A, Tropini C, et al. (2019) Recovery of the Gut Microbiota after Antibiotics Depends on Host Diet, Community Context, and Environmental Reservoirs. Cell Host Microbe. 26(5):650-665.e4.
- Müller C. (2023) Mikrobiom. Der Darm und seine Bewohner. Bundeszentrum für Ernährung. Verfügbar unter: https://www.bzfe.de/ernaehrung/ernaehrungswissen/gesundheit/mikrobiom/ [zitiert am 9. April 2024]
- Paas D. (2013) Ursachen für Verdauungsprobleme. Ernähr Med. 28(03):120–3.
- Slavin J. (2013) Fiber and Prebiotics: Mechanisms and Health Benefits. Nutrients. 5(4):1417–35.
- Sanders ME, Merenstein DJ, Reid G, et al. (2019) Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nat Rev Gastroenterol Hepatol. 16(10):605–16.
- FitzGerald J, Patel S, Eckenberger J, Guillemard E, et al. (2022) Improved gut microbiome recovery following drug therapy is linked to abundance and replication of probiotic strains. Gut Microbes. 14(1):2094664.
- Şanlier N, Gökcen BB, Sezgin AC. (2019) Health benefits of fermented foods. Crit Rev Food Sci Nutr. 59(3):506–27.
- Butel MJ. (2014) Probiotics, gut microbiota and health. Médecine Mal Infect. 44(1):1–8.
- Kalakuntla AS, Nalakonda G, Nalakonda K, et al. Probiotics and Clostridium Difficile: A Review of Dysbiosis and the Rehabilitation of Gut Microbiota. Cureus. 11(7):e5063.
- Österreichische Gesellschaft für Ernährung (2021) Ernährung von A-Z. Präbiotika. Verfügbar unter: https://www.oege.at/category/ernaehrung-von-a-z/#praebiotika [zitiert am 9. April 2024]
- Bundesministerium für Ernährung und Landwirtschaft (2021) Kompass Ernährung. Gutes Bauchgefühl. Gesundheit beginnt im Darm.
- Stephen AM, Champ MMJ, Cloran SJ, et al. (2017) Dietary fibre in Europe: current state of knowledge on definitions, sources, recommendations, intakes and relationships to health. Nutr Res Rev. 30(2):149–90.
- Reid G, Younes JA, Van Der Mei HC, et al. (2011) Microbiota restoration: natural and supplemented recovery of human microbial communities. Nat Rev Microbiol. 9(1):27–38.